Abstract
Background
Myeloid-derived suppressor cells (MDSC) contribute to an immunosuppressive tumor environment and are a barrier to immune therapeutic approaches, including cell-based therapies such as chimeric antigen receptor T cells (CAR T). Despite good overall response rates with certain subsets of B cell leukemias and lymphomas, a significant percentage of patients treated with CAR T therapy do not respond or subsequently relapse. Poor CAR T expansion, poor persistence of infused cells, and clinical treatment failure are associated with tumor and systemic immune dysregulation including high blood levels of peripheral blood monocytic MDSC (M-MDSCs) and interleukin-6, both of which are associated with lack of durable responses 1. In addition, CAR T therapy has been limited by the occurrence of severe cytokine release syndrome (CRS), which is associated with high IL-6 production 2 by myeloid cells such as MDSC.
AMV564 is a potent T cell engager that selectively depletes MDSC while promoting T cell activation and proliferation without significant IL-6 induction 3. In phase 1 studies in acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and solid tumors, AMV564 has been demonstrated to be clinically safe and active with some patients achieving complete remissions.
Methods
Cell lines, primary human cells, and patient samples were analyzed using flow cytometry with appropriate marker panels. T cell activation and cytotoxicity assays were conducted using primary human T cells from healthy donors and target cells (3:1 ratio) for 72 hours. T cell activation using ImmunoCult Human CD3/CD28 served as an assay reference.
Results
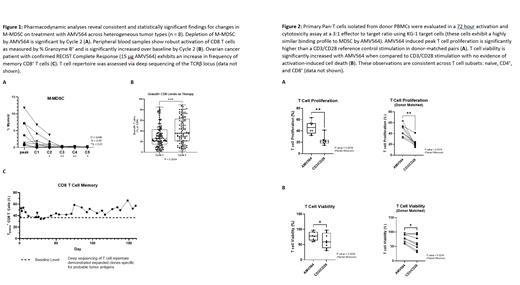
Analysis of patients treated with AMV564 demonstrated statistically significant selective depletion of M-MDSC by cycle 2 (Fig. 1A). While on AMV564 therapy, median IL-6 levels remained below 100 pg/mL despite robust T cell activation and expansion. Granzyme B production by CD8 T cells increased significantly between Cycle 1 and Cycle 2 in patients on therapy, and effector CD8 T cells expand over the course of treatment (Fig. 1B-C). These data collectively support the finding that AMV564 both removes a key source of immune suppression and is a potent agonist of T cell function and differentiation in patients.
AMV564 potently activates and expands primary T cells ex vivo. Across donors, peak proliferation was significantly higher with AMV564 than with the CD3/CD28 reference (Fig. 2A). Importantly, T cell viability remained significantly higher with AMV564 when compared to reference control (CD3/CD28), and there was no evidence of activation-induced cell death (AICD) in AMV564-treated samples (Fig. 2B).
Conclusions
AMV564 depletes MDSC and stimulates expansion and longevity of T cells without significant IL-6 induction, suggesting a possible strategy for improvement in efficacy of cell-based therapy such as CAR T approaches. As circulating M-MDSC both at baseline and after CAR T infusion correlate with poor clinical efficacy 4, AMV564 may have beneficial effects during the conditioning phase of cell therapy, after re-infusion of CAR T products into patients, or both. Ex vivo studies using donor T cells and ongoing in vitro studies using CAR T molecules suggest that AMV564 may provide dual benefit with respect to both depletion of MDSC and T cell agonism.
References
1. Jain, et al; Blood 2021; 137 (19): 2621-2633. doi: https://doi.org/10.1182/blood.2020007445
2. Li et al., Sci. Transl. Med. 11, eaax8861 (2019)
3. Eckard et al; Cancer Res 2021; (81) (13 Supplement) 528; DOI: 10.1158/1538-7445.AM2021-528
4. Jain, et al; Blood 2019; 134 (Supplement_1): 2885. doi: https://doi.org/10.1182/blood-2019-131041
Eckard: Amphivena Therapeutics: Current Employment. Rojo: Amphivena Therapeutics: Current Employment. Smith: Amphivena Therapeutics: Current Employment. Chun: Amphivena Therapeutics: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal